General Information about Breast Cancer
Breast cancer is a type of cancer that forms in tissues of the breast, usually the ducts (tubes that carry milk to the nipple) and lobules (glands that make milk). It occurs in both men and women, although male breast cancer is rare. Breast cancer is the most common type of cancer among women in this country (other than skin cancer). Each year, over 200,000 American women are diagnosed with this disease.
Signs and Symptoms of Breast Cancer
Symptoms of breast cancer may include: a lump or thickening in or near the breast or in the armpit area, nipple tenderness, a change in how the breast or nipple appears, a change in the size or shape of the breast, a change in the skin of the breast or nipple, and nipple discharge (fluid).
Early breast cancer usually does not cause pain. However, a woman should see her health care provider about breast pain or any other symptom that does not go away after a few weeks. Any woman with these symptoms should be evaluated by a physician as soon as possible.
Helpful Terms Regarding Breast Cancer
- BB's - Small markers that are placed on the skin for localization purposes during radiation therapy.
- Blocks - Used for some patients' treatments to block out unnecessary structures within the treatment field (heart, lung, etc.).
- Dry desquamation - Dryness, itching, scaling, flaking and peeling of the skin.
- Ductal carcinoma in situ (DCIS) - Abnormal cells in the lining of a duct which is considered non-invasive disease. The abnormal cells have not spread outside the duct or invaded the nearby breast tissue. DCIS can become invasive cancer if not properly treated
- Ecchymosis - A bruise or contusion.
- Erythema - Abnormal redness and inflammation of the skin.
- Fat necrosis - Necrosis of adipose tissue, characterized by the formation of small quantities of calcium soaps when fat is hydrolyzed into glycerol and fatty acids. Also known as steatonecrosis.
- Gantry - The C-arm part of the linear accelerator that rotates around you to deliver radiation from different angles.
- HDR (High Dose Rate) Brachytherapy - Implantation of a temporary high dose rate pellet which delivers radiation to a specific site in the body.
- Induration - Hardening and swelling of a part of the body.
- Lasers - Red lasers in the treatment room that the therapists will use to align you in the correct treatment position.
- Linear Accelerator - The machine that delivers the radiation treatment.
- Lumpectomy - Surgical removal of the breast tumor alone.
- Lymph node dissection - Surgical removal of lymph nodes, in breast cancer the lymph nodes in the armpit (axilla) are dissected. Often times a sentinel lymph node biopsy is done first.
- Lymphedema - The accumulation of fluid in soft tissues of the body with accompanying swelling, often of the extremities: sometimes caused by inflammation, obstruction or removal of lymph channels.
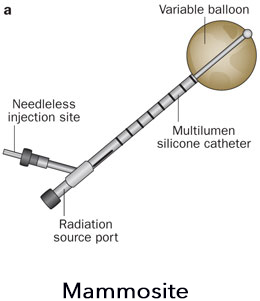
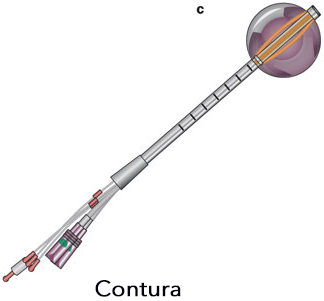
- MammoSite/Savi/Contura - Brand names of breast implants/balloons which are inserted into the lumpectomy bed for targeted radiation therapy for breast cancer.
- Mastectomy - Surgical removal of the all breast tissue in the affected breast.
- Metastasis - The spread of malignant or cancerous cells to other parts of the body by way of blood or lymphatic vessels or membranous surfaces.
- Moist desquamation - Moist peeling of the skin which sometimes can be associated with blistering.
- Port films - X-ray films that confirm the treatment area and patient positioning (taken on a weekly basis for treatment quality assurance purposes).
- Pruritus - Itching
- Sentinel Lymph node biopsy - A tracer or dye that is injected into the breast where the tumor originates, it then drains into the axilla (armpit) to help guide the surgeon to which lymph nodes need to be sampled. This procedure reduces the risk of lymphedema in comparison to a lymph node dissection.
- Seroma - A mass or swelling caused by the localized accumulation of serum (fluid) within a tissue or organ. These normally absorb on their own, however it sometimes may require surgical drainage.
- Stage 0 is carcinoma in situ.
- Lobular carcinoma in situ: Abnormal cells in the lining of a lobule which is considered non-invasive disease. However, LCIS does indicate an increased risk of invasive breast cancer.
- Ductal carcinoma in situ (DCIS): Abnormal cells are in the lining of a duct which is considered non-invasive disease. The abnormal cells have not spread outside the duct or invaded the nearby breast tissue. DCIS can become invasive cancer if not properly treated.
- Stage I is the earliest stage of invasive breast cancer.
- The tumor is no more than 2 centimeters (three-quarters of an inch) across. Cancer cells have not spread beyond the breast.
- Stage II - is one of the following:
- The tumor is no more than 2 centimeters (three-quarters of an inch) across. The cancer has spread to the lymph nodes under the arm.
- The tumor is between 2 and 5 centimeters (three-quarters of an inch to 2 inches). The cancer has not spread to the lymph nodes under the arm.
- The tumor is between 2 and 5 centimeters (three-quarters of an inch to 2 inches).
- The cancer has spread to the lymph nodes under the arm.
- The tumor is larger than 5 centimeters (2 inches).
- The cancer has not spread to the lymph nodes under the arm.
- Stage III is locally advanced cancer. It is divided into Stage IIIA, IIIB, and IIIC.
- Stage IIIA is one of the following:
- The tumor is no more than 5 centimeters (2 inches) across. The cancer has spread to underarm lymph nodes that are attached to each other or to other structures. Or the cancer may have spread to lymph nodes behind the breastbone.
- The tumor is more than 5 centimeters across. The cancer has spread to underarm lymph nodes that are either alone or attached to each other or to other structures. Or the cancer may have spread to lymph nodes behind the breastbone.
- Stage IIIB is a tumor of any size that has grown into the chest wall or the skin of the breast. It may be associated with swelling of the breast or with nodules (lumps) in the breast skin.
- The cancer may have spread to lymph nodes under the arm.
- The cancer may have spread to underarm lymph nodes that are attached to each other or other structures. Or the cancer may have spread to lymph nodes behind the breastbone.
- Inflammatory breast cancer is a rare type of breast cancer. The breast looks red and swollen because cancer cells block the lymph vessels in the skin of the breast. When a doctor diagnoses inflammatory breast cancer, it is at least Stage IIIB, but it could be more advanced.
- Stage IIIC is a tumor of any size. It has spread in one of the following ways:
- The cancer has spread to the lymph nodes behind the breastbone and under the arm.
- The cancer has spread to the lymph nodes above or below the collarbone.
- Stage IV is distant metastatic cancer. The cancer has spread to other parts of the body.
Recurrent cancer is cancer that has come back (recurred) after it has been treated. It may recur locally in the breast or chest wall. However, it may also recur distantly in any other part of the body, such as the bone, liver, or lungs.
Treatment of Breast Cancer
To plan your treatment, your doctor needs to know the extent (stage) of the disease. The stage is based on the size of the tumor and whether the cancer has spread. When breast cancer spreads, cancer cells are often found in lymph nodes in the axilla (armpit). The stage often is not known until after surgery to remove the tumor in your breast and the lymph nodes in your axilla. Staging may also involve imaging tests and lab tests. These tests can show whether the cancer has spread and, if so, to what parts of your body.
Breast cancer treatment often requires both local and systemic therapy:
Local Therapy
Surgery is always required for definitive local treatment. This removes the bulk of the tumor which can then be analyzed by a pathologist.
Radiation is added after lumpectomy to prevent any cancer relapse in the breast. Sometimes after mastectomy, radiation is recommended if high risk features are found.
Systemic Therapy
Some women with higher risk disease may need systemic therapy after local therapy to prevent the cancer from coming back in the body. Chemotherapy, hormonal therapy, and biological therapy are systemic treatments. They enter the bloodstream and destroy or control cancer throughout the body. Some women with breast cancer have systemic therapy to shrink the tumor before surgery or radiation.
Surgery
Therapeutic Surgery
Both breast-sparing (lumpectomy) and mastectomy surgeries are options for patients with breast cancer. Surgery is often followed with radiation and chemotherapy treatments to prevent any future relapse.
Reconstructive Surgery
We work closely with skilled plastic surgeons who can evaluate you for breast reconstruction if necessary. This multi-disciplinary approach ensures the best cosmetic outcome and chance for curing your breast cancer.
Radiation Therapy
External beam radiation delivers radiation via a source outside or external to the body, in this case through a linear accelerator machine. This complex machine uses electricity to produce high-energy x-rays, targeted and delivered to the affected breast. These x-rays deposit the prescribed dose of radiation deep within the body while sparing surrounding structures.
The actual radiation treatment is invisible, tasteless, odorless, and painless. External beam radiation is a completely non-invasive technique. It works by damaging cancer cells and slowing their ability to grow and divide. Healthy cells can repair the effects of radiation fairly quickly while cancer cells have a difficult time recovering. By delivering radiation over a pre-determined amount of time (approximately 6-8 weeks), we allow the healthy tissues to repair while repeatedly damaging the cancer cells.
LINAC External Beam Radiation Treatment
Delivered by our state-of-the-art linear accelerator machine, beams of radiation are carefully aimed directly at the affected breast. The linear accelerator machine uses on board imaging to monitor the position and movement of the breast, ensuring that the surrounding healthy tissue is not affected.
High Dose Rate (HDR) Brachytherapy
HDR Brachytherapy for Breast cancer is a procedure that involves surgically placing an implant within the tumor bed of the lumpectomy site. Once the implant is placed, a small radioactive source (Iridium-192) is temporarily placed within multiple areas of the implant. The use of such implants can deliver radiation doses to areas that may contain residual cancer after your lumpectomy. This form of treatment can be used as a primary course of treatment or can be combined with External Beam Radiation Therapy (EBRT). Candidates of this procedure will be determined by your radiation oncologist.
Although the overall structure of each implant may differ, the basic principles and course of treatment are relatively similar. The first step of HDR brachytherapy is placing a deflated balloon implant into the breast during or after the lumpectomy. The device is then expanded into the tumor bed and remains in the patient throughout the course of treatment. At this time the medical dosimetrist and radiation oncologist will formulate a treatment plan that accounts for each patient's unique anatomy. The implant is then connected to an HDR afterloader that permits the radioactive source to travel in and out of the device. This same treatment will be repetitively done throughout the course of a week. Once the prescribed dose has been administered, each implant is deflated and removed from the patient.
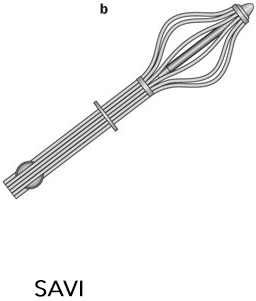
SAVI Multi-Lumen Radiation Implant Application
Developed by Cianna Medical, the SAVI is a strut-based implant with multiple lumens. The multiple lumen structure permits the medical dosimetrist and radiation oncologist the ability to optimally deliver a prescribed dose while sparing the healthy surrounding structures. The SAVI's structure differs from comparable implants since the struts open directly into the tissue rather than an expanding balloon.

Expanded and Collapsed SAVI
SenoRx's Multi-Lumen Radiation Balloon Application
SenoRx has developed Contura™, a multi-lumen radiation balloon applicator for accelerated partial breast irradiation. The radiation balloon uses a vacuum to remove excess fluid and to adhere closely to often irregularly shaped lumpectomy cavities in order to deliver precise radiation dosing through multiple seed lumens. This is a form of HDR brachytherapy. Treatment time is reduced to days versus weeks. The accurate and targeted radiation dosing decreases potential recurrence of cancer cells in the lumpectomy site.

Expanded Contura Implant
MammoSite® and Interstitial Localized Short Course Radiation
After the breast tumor is removed, a small soft MammoSite balloon attached to a catheter is placed inside the lumpectomy cavity under ultrasound guidance. Small radioactive seeds are then inserted into the catheters by a computer-controlled HDR (High Dose Rate) afterloader machine for accuracy of dosage and placement. The catheter and balloon are then easily removed on the last day of treatment, leaving no radiation inside the breast.

Expanded MammoSite Implant
Varian GammaMed Plus iX Remote Afterloader
The Varian GammaMed Plus iXdelivers HDR radiation treatments based on times calculated by the medical dosimetrist and physician. The machine contains a radioactive source called Iridium 192. The source, approximately 5mm long, is attached to a long cable that is also contained in the machine. The machine, housed in a special treatment room called the HDR vault, is linked to a computer controlled by the physician delivering the treatment. The radiation therapist stands outside the HDR vault and monitors the patient undergoing treatment. This is used on conjunction with the Savi, Contura or MammoSite implant.

Chemotherapy (Medical Oncology)
Chemotherapy usually includes a combination of drugs (taken orally or intravenously, to kill or slow the growth of rapidly multiplying cancer cells. These drugs travel throughout the body to rid cancer cells which may have escaped into the blood stream. We work closely with medical oncologists, and CCOI will make the necessary arrangements for you to be evaluated for chemotherapy if necessary.
Frequently Asked Questions
Q: What do I need to bring when I come to the Cancer Center of Irvine for treatment?
A: If you are interested in coming to the Cancer Center of Irvine for treatment, you first need to call 949.417.1100 to schedule an appointment. Here is a list of things to bring when you come in for the first time:
Medical records from physicians involved in the care of your breast cancer.
- Recent doctor notes
- Recent labs
- Recent pathology
- Imaging (Mammogram, Ultrasound, Bone Scans, MRI, CT, PET)
- Insurance card(s)
- Forms - Upon calling the Cancer Center, a packet of forms will be mailed to you along with a map to our facility.
External Radiation FAQ
Q: What are the common side effects of breast irradiation and when shall I expect them to appear?
A: The actual radiation treatments are painless; however, the side effects may bother you. Common side effects are redness and irritation of the skin in the area being treated. Some patients may experience skin dryness, tingling, throbbing, peeling, and discoloration in the treated area. Skin reactions may appear within 2 weeks of treatments. However, each patient's reactions are unique. Side effects are reversible and usually subside in 2-3 months after treatment.
Q: What can I do to alleviate skin irritation?
A: We recommend that during the course of radiation the patient apply alcohol-free 100% aloe vera gel and/or Aquaphor cream. If there is moist peeling some patients may need a special antibiotic cream. Wear loose cotton clothing.
Q: What are tattoos and why are they needed?
A: The tattoos are small permanent marks placed on the skin surface with a needle and India ink. The therapists refer to these tattoos for treatment positioning and radiation field alignment.
Q: Can I shave my underarm?
A: Do not shave the underarm of the area being treated. Skin is sensitive in that area during the radiation treatments and shaving will irritate that area.
Q: What will I feel during the treatment?
A: You will not feel or see anything during treatment. However, you will hear a buzzing noise while the radiation beam is on.
Q: Why am I feeling tired?
A: Fatigue is a common side effect of radiation, usually experienced two weeks into treatment. However, every patient is different and fatigue levels will vary. The fatigue is reversible and usually subsides 3-4 weeks after finishing radiation treatment.
Q: What if I need to miss a day of treatment?
A: Missing a day of treatment is permissible, however, all absences should be cleared with the doctor or radiation therapist first. The missed treatment will be made up with an additional treatment at the end.
Q: What diet should I be on during radiation treatments?
A: In general, there are no diet restrictions with radiation to the breast.
Brachytherapy FAQ
Q: Now that I have been scheduled for placement of the device, what happens next?
A: Your treatments will start the same day you have the device placed by the breast surgeon. You will come directly to the Cancer Center of after your surgery, so we can begin your treatments. Please give us a call when you are on your way so we will be ready for you. 949.417.1100
Q: Will I be able to drive myself?
A: On your first day, you may wish to have someone drive you because you will have received anesthesia from the surgery. After your first day, you are safe to drive yourself as long as you are not taking strong narcotic pain medication.
Q: Are there any restrictions on what to wear during the course of my brachytherapy treatments?
A: Do not wear bras with underwire during the course of your treatments. Blouses/tops that open in the front are preferred in order to provide easy access to the catheter. Sports bras that open in the front are also recommended. These bras can be found at most clothing stores (Walmart, Target, etc.)
Deodorant is allowed as long as it does not contain aluminum or alcohol. Tom's of Maine and Crystal both make safe options. You may find them at Wal-Mart, Target, Trader Joe's, etc.
Q: What will happen when I arrive at the center?
A: You will have a CT scan for the planning of your treatment. No preparation, needles or injections are necessary. You will be in the CT room no longer than 30 minutes.
Q: When will I have my first treatment?
A: There will be a 30 to 90 minute wait after the CT scan, while your radiation treatment is being planned, after which you will have your first treatment. While you wait, you may relax in our lobby and help yourself to refreshments.
Q: How long do the treatments take?
A: Each treatment takes about 15 minutes. The radiation therapist will also change your dressing each time.
Q: Do I get a CT scan every day?
A: Yes, before each treatment, but it only takes 5 minutes. This is for your protection, to make sure that the device is in the same position as it was originally planned with.
Q: When are my appointments?
A: We play the first day "by ear" depending on when you get here, treatment planning time, etc. But for the following four days, your twice-daily appointments are scheduled early to allow a six hour window between treatments. For example: 8 a.m. & 2 p.m. or 8:30 a.m. & 2:30 p.m.
Q: Who will be delivering the treatments?
A: Our staff consists of five men and women specially trained in radiation therapy. Your therapist may vary due to a scheduling. If you have any questions or concerns regarding this, please let us know before we begin your treatment.
Q: Can I bring someone to watch the treatments?
A: For the initial treatment it is fine for a family member/friend to watch the treatment in order to see how to take care of the dressing. We ask that this person does not accompany you for the remaining treatments. The treatment area is in a "patient zone" and in order to respect the privacy of others we ask that your companions remain in our lobby.
Q: When will I be able to shower?
A: We ask that you wait 24 hours after the surgery.
Q: What happens after my last treatment?
A: Either our nurse or physicians will remove the device. No stitches are necessary; all that is needed is Neosporin and gauze. These will be applied until the incision site heals (usually for 1-2 days). We also recommended you take Aleve, Extra Strength Tylenol or Advil about 30 minutes before the last treatment.
Q: What comes next?
A: Your radiation oncologist will want to see you for a follow-up exam on the next office day following your last treatment. The follow-up exam will only take about 15 minutes.
A Tip For You
There will be a lot of drainage at the incision site, so don't be alarmed. This drainage is a good thing. The radiation therapist will change your dressing during each treatment and show you what you need to do. You will need Neosporin at home when you change the dressing. Besides gauze, a Kotex pad works great to absorb excess drainage.

